Ammalife is lucky to support a team of talented researchers in Malawi who are seeking practical, low-cost and low-resource solutions to preventing, diagnosing and treating maternal sepsis. In the first of this two-part blog series we speak to Catherine Dunlop, a Research Fellow at Birmingham University, who is currently undertaking a PhD research project on preventing maternal infection and sepsis.
I’m a doctor by trade with a special interest in preventing maternal deaths and for the last few months I’ve been in the field in Malawi, working with the FAST-M team. Specifically, the project focuses on preventing infection which is the first stage along the path to sepsis. I’ve already finished the first part of the project, which involved conducting baseline assessments of the needs of the hospitals and interviewing staff members on the project sites. The second stage of the project involved training and implementation. I’m now in the final stage of the project, monitoring and evaluation of the project to see if the project has had any impact on decreasing rates of infection, and we are hoping for encouraging results!
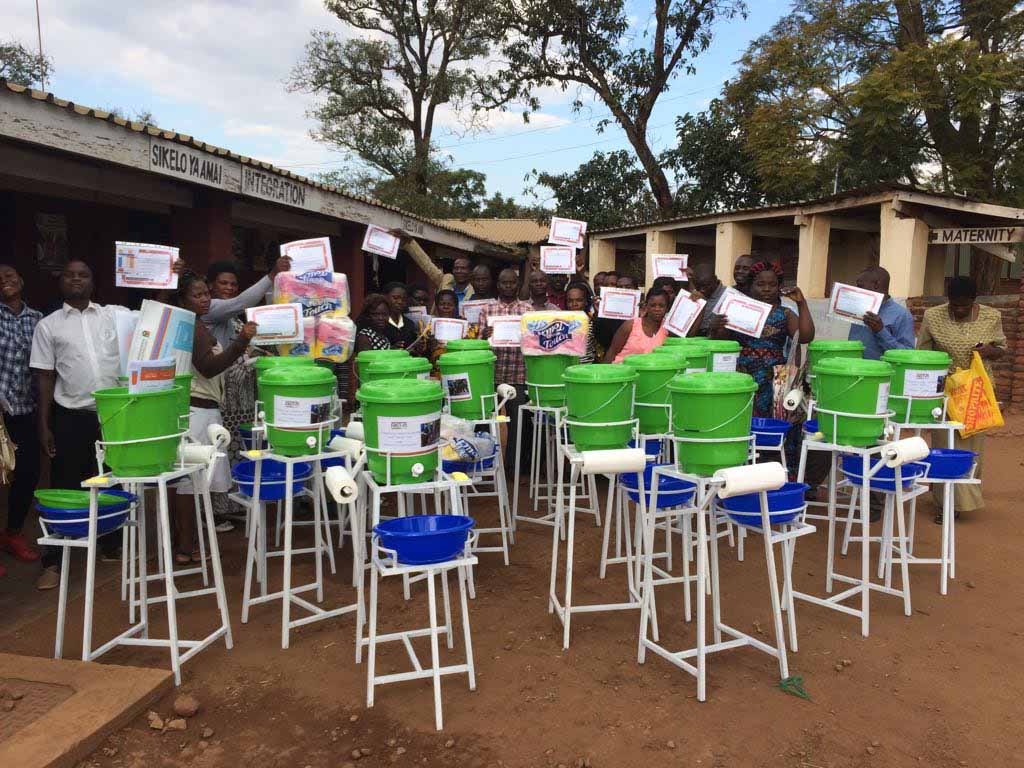
- Catherine (far left, middle row) and the training participants outside Kabudula Community Hospital
- One of the new hand washing stations provided for the FAST-M Sepsis Project
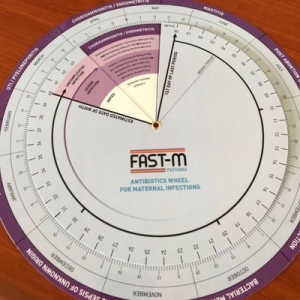
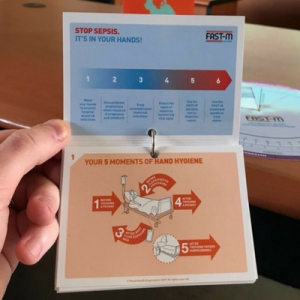
Sepsis is one of the three main causes of maternal mortality across the world, together with postpartum haemorrhage (PPH) and eclampsia. It’s caused by infection, often through poor hygiene practices, which is why we we’re seeking practical solutions to stop the root causes of infection. There are three components to the infection prevention branch of FAST-M, which I have been implementing as part of my research. The first element consists of promoting good hand-washing and hand hygiene practices to stop the spread of infections in the hospital, especially during key moments such as during Caesarean sections. We recently had a huge delivery of standalone hand-washing stations at one of the hospitals to enable hand-washing and we’ve also introduced alcohol gels. Secondly, we’ve been rolling out the World Health Organisation (WHO) recommendations for preventing maternal infections, distributing posters and booklets, which has been accompanied by training. The third and final element of the project has been to introduce the FAST-M wheel tool to help clinicians decide which antibiotics to administer in case of infections, as there are many different types of infection that can lead to sepsis. In addition to these three steps we also devised a hand hygiene dance incorporating the different stages of hand-washing as a fun way to help participants remember what they had learnt!
On a typical day in the study I normally spend half of my time on one of the three project sites and half the time back at my own base doing data analysis. In the mornings I usually visit one of the hospitals to attend morning meetings and to speak with the staff. I also attend hand hygiene observations with the FAST-M project officers once a week and it’s during these sessions that resources for the upcoming week are also distributed. We also frequently visit the wards to give verbal feedback to the clinicians on the study results so far. I’ve been working closely with both the FAST-M Project Coordinator, Laura Munthali, and the Project Officer, Harry Liyaya, who are permanently based in Malawi and who keep the project running smoothly.
- The FAST-M Antibiotics Wheel Tool enables clinicians to decide which antibiotics to use to treat mothers with various different types of infections
- The WHO Sepsis Prevention Recommendations were disseminated as part of Catherine’s work and the FAST-M Project
I’m really enjoying my time here in Malawi but there are certainly obstacles to overcome when conducting an international study! The unreliable internet connection is one of the main challenges, and often the power supply is unstable; in fact last week I received a warning that there would be no power supply in the upcoming weekend, so I had to ensure that I had everything charged. Nevertheless, my phone charge pales in comparison to some of the challenges facing the practitioners in Malawi, who are constantly battling against a lack of resources. Still, I’ve been impressed with just how devoted the doctors and clinicians in Malawi are to improving the quality of care for their patients.